Congress highlights: NMIBC
In this section
How can clinicians select the best option for patients with non-muscle-invasive bladder cancer (NMIBC) that does not respond to Bacillus Calmette–Guérin (BCG)? Here, we round up the discussions and key data from the 2025 American Society of Clinical Oncology (ASCO) Genitourinary (GU) Cancers Symposium.
We also highlight research in intermediate-risk NMIBC, and Neal Shore (Carolina Urologic Research Center, Myrtle Beach, South Carolina, USA) discusses what the latest findings may mean for the care of patients with NMIBC.
Neal Shore discusses “the art of medicine” required to ensure maximum benefit from BCG maintenance therapy for patients with NMIBC in the face of multiple challenges. View transcript.
BCG-unresponsive NMIBC: Where next?
A key session on NMIBC addressed the question of which treatment to select for patients with BCG-unresponsive disease, with an expert panel talking through the options for a real-world patient case.
Session Co-Chair Bogdana Schmidt (Huntsman Cancer Institute at the University of Utah, Salt Lake City, USA), summarized the challenge, saying: “When there’s a small menu, you pick what you have. When there’s a larger menu, you have to think back to what do patients want and what can we do to meet their needs.”
Given all the options now becoming available, the “impressive” early efficacy of some of these in BCG-naive patients with high-risk disease, and the potential for highly individualized treatment using biomarkers and targeted therapies, Schmidt believes that BCG monotherapy “is not the way of the future.”
The panel rounded up the efficacy, safety, and treatment burden considerations for pembrolizumab, alone and combined with radiation therapy; for the interleukin-15 superagonist nogapendekin alfa inbakicept; and for the nonreplicating adenoviral vector-based gene therapy nadofaragene firadenovec.
The last of these options was approved around 2 years ago, and this year’s ASCO GU saw the first presentation of real-world data for the treatment, by Jacob Moyer (Graduate School of Biomedical Sciences, Phoenix, Arizona, USA) and colleagues. This showed positive outcomes in line with the efficacy seen in the clinical trials.
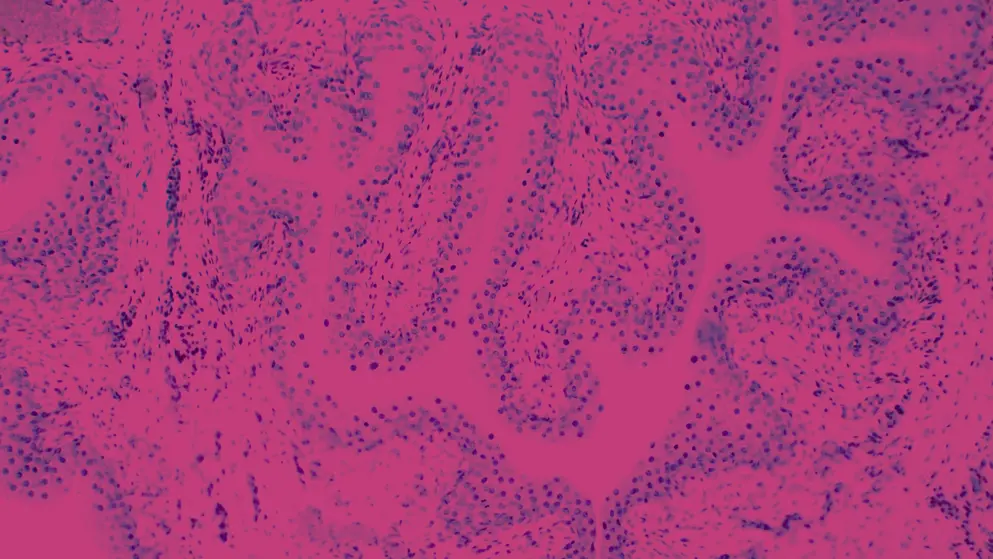
The 24 patients in the study had carcinoma in situ (CIS) with or without papillary disease. They were an average age of 71 years, 63% had prior intravesical chemotherapy, 26% had prior pembrolizumab treatment, and the median time from diagnosis to nadofaragene firadenovec treatment was 33 months.
At 3 months, 79% patients had a complete response (CR), with 84% of these maintaining CR at a median follow-up of 7.3 months. The most common adverse event (AE) was grade 1–2 bladder spasms (61%); just four patients experienced a grade 3 AE – two with fatigue, one with fever, and one with dizziness.
Does the real-world performance of nadofaragene firadenovec live up to its clinical trial promise? Shore gives his view and explains the rationale for assessing it in patients with intermediate risk. View transcript.
Returning to the panel discussion, despite the positive safety data supporting the available non-surgical options for BCG-unresponsive disease, for the specific case in question, the experts remained in favor of radical cystectomy based on the patient’s age and high-risk features (T1 disease plus CIS after progressing on gemcitabine and docetaxel). They proposed chemoradiation therapy or enrollment in a clinical trial as a back-up if the patient refused cystectomy.
Emerging therapies: An “exciting time”
The treatment menu for BCG-unresponsive NMIBC seems set to expand further, with panelist Girish Kulkarni (Princess Margaret Cancer Centre, Toronto, Ontario, Canada) highlighting the “diverse” mechanisms of action of in-development treatments, and saying that now is “an exciting time for all of us.”
The panelists highlighted several options with previously reported promising early data, namely:
- An intravesical delivery system known as “the pretzel,” which releases 225 mg gemcitabine over 21 days – tested in the SUNRISE-1 trial
- The non-viral intravesical gene therapy detalimogene voraplasmid, showing encouraging data in the LEGEND trial
- The intravesical, conditionally replicating virus cretostimogene grenadenorepvec, assessed as monotherapy in BOND-003 and in combination with pembrolizumab in CORE-001
Another potential treatment approach for BCG-unresponsive, high-grade NMIBC is the PD-L1 inhibitor durvalumab plus intravesical gemcitabine and docetaxel, which is being tested as part of the ADAPT-BLADDER trial. Noah Hahn (Johns Hopkins University Sidney Kimmel Comprehensive Cancer Center, Baltimore, Maryland, USA) presented the phase 1/2 findings, involving a total of 40 patients.
The study participants received up to six cycles of durvalumab 1,500 mg every 4 weeks plus weekly intravesical gemcitabine 1,000 mg and docetaxel 37.5 mg. Monthly gemcitabine/docetaxel maintenance was recommended for patients with a CR.
Just 5% of the cohort had grade 3 AEs – two cases of pneumonitis and one of dyspnea – and there were no grade 4 AEs. One death occurred, which was considered unrelated to study treatment.
Overall, 89.2% of 37 evaluable patients had a CR, comprising 90.0% of 20 participants with CIS and 88.2% of 17 with pure papillary disease. Of the 16 patients evaluable at 12 months, 68.8% maintained a CR and 31.3% had recurrence.
"This is taking a proactive, some might argue a slightly more aggressive, approach." Shore discusses how therapeutic combinations including immune checkpoint inhibitors (ICIs) and chemotherapy might benefit patients, especially those with high-risk disease. View transcript.
UGN-102 for intermediate-risk NMIBC
Elsewhere at the conference, two posters presented by Sandip Prasad (Morristown Medical Center, New Jersey, Florida, USA) and team provided additional data from the phase 3 ENVISION and ATLAS trials. These tested UGN-102, a reverse thermal hydrogel containing mitomycin, administered as a monotherapy in ENVISION and in combination with transurethral resection of bladder tumor (TURBT) in patients with recurrent low-grade intermediate-risk NMIBC in ATLAS.
How might intravesical drug delivery systems influence clinical decision-making, and could they even affect decisions around TURBT? Shore offers his view. View transcript.
The latest findings show that the probability of maintaining a CR at 12 months was 82.3% in ENVISION and 79.7% in ATLAS. The probability with TURBT alone (in ATLAS) was 67.7%, equating to a significant 54% reduction in recurrence risk for ATLAS participants who also received UGN-102.
The most common AE was dysuria, occurring in about 20–30% of participants.
The researchers also reported that neither focality nor tumor burden significantly impacted the likelihood of CR at 3 months. As assessed in a subanalysis of ENVISION, CR rates were 79.3% and 82.9% in patients with multiple and single tumors, respectively, and were 82.8% and 73.2% in those with tumor burden of no more than 3 cm or greater than 3 cm, respectively.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.
of interest
are looking at
saved
next event

